Mild Traumatic Brain Injuries (mTBI): The Injury You Can’t Always See
Every year, an estimated 42 million people worldwide suffer a mild traumatic brain injury — what most of us casually call a concussion. That number alone is staggering. In the United States, more than 1% of the population sustains a reported mTBI each year. But the true scope of the problem is even larger.
Researchers estimate that up to 50% of mild TBIs go undocumented, meaning millions of brain injuries are never formally diagnosed or recorded. Many people are treated briefly in an emergency room, urgent care clinic, or primary care office and sent home. Others never seek treatment at all, assuming they are “fine.”
And that’s the danger. When a brain injury is minimized, overlooked, or underreported, the opportunity for proper monitoring, treatment, and recovery can be lost — and the long-term consequences may not show up until much later.
What Causes a Traumatic Brain Injury?
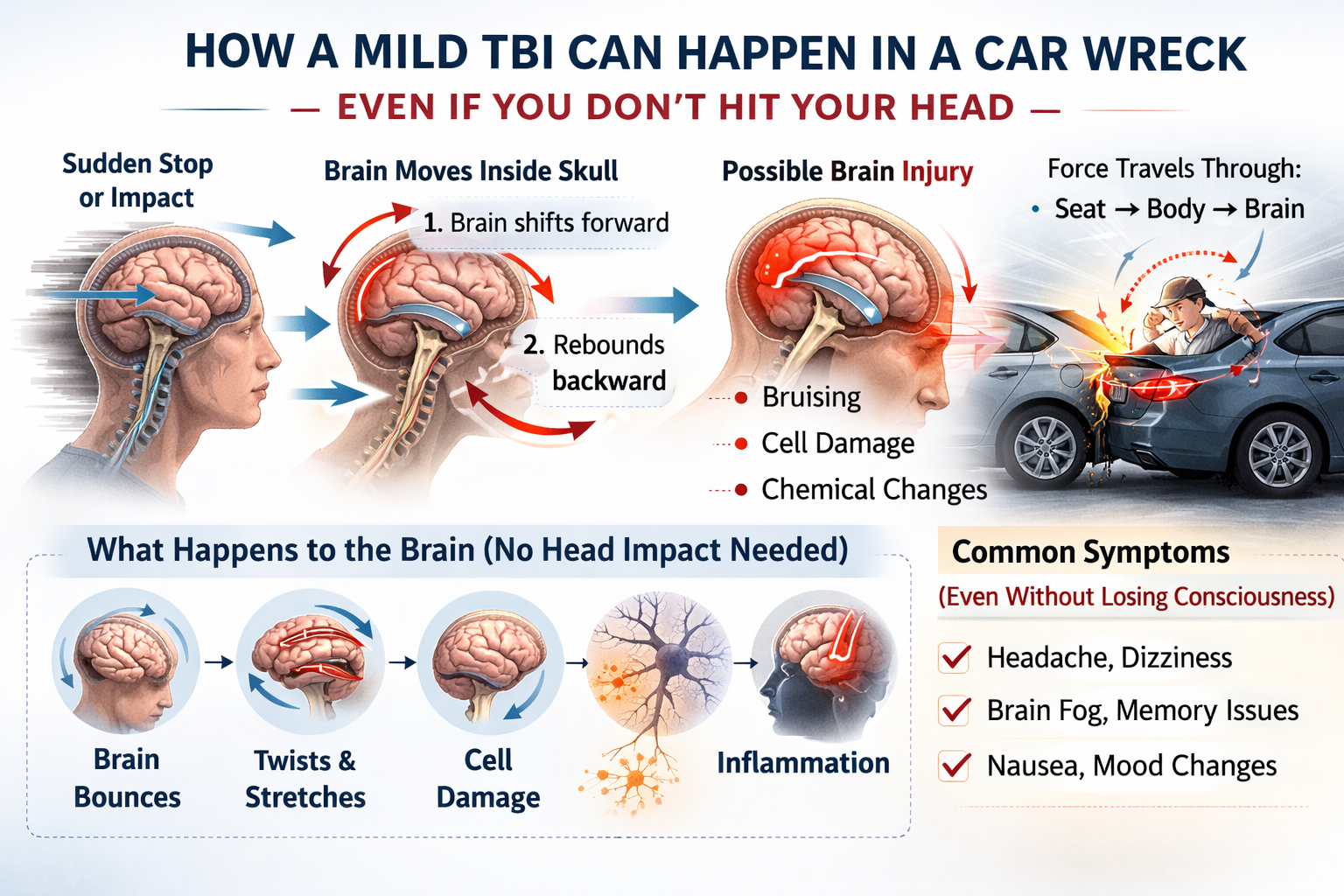
A mild traumatic brain injury occurs when a bump, blow, or jolt to the head — or a forceful hit to the body — causes the brain to move rapidly back and forth inside the skull. In a car wreck, this can happen even if you never strike your head on the steering wheel, window, or dashboard. The sudden acceleration and deceleration forces alone can cause the brain to shift inside the skull, creating injury without any visible impact.
That sudden movement can cause the brain to:
- Bounce against the skull
- Twist inside the cranial cavity
- Stretch and damage brain cells
- Trigger chemical changes in the brain
Even when there is no loss of consciousness, and even when there is no visible bruise or laceration, the brain can still be injured.
How Doctors Classify Traumatic Brain Injuries?
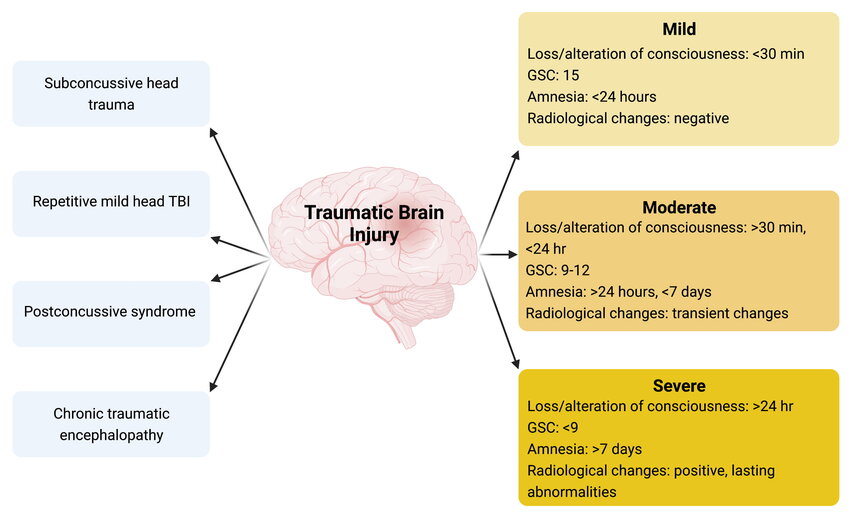
Traumatic brain injuries are generally classified as mild, moderate, or severe based on factors like loss of consciousness, memory disruption, neurological symptoms, and imaging findings. A mild TBI (concussion) may involve brief confusion, dizziness, headache, or memory gaps — and often occurs without loss of consciousness. A moderate TBI typically involves a longer period of confusion or unconsciousness and more noticeable cognitive or physical impairment. A severe TBI usually includes extended loss of consciousness, significant neurological deficits, and may result in permanent disability. Importantly, the term “mild” refers to the initial presentation — not the long-term impact. Even a so-called mild TBI can have serious and lasting consequences.
Related Brain Injury Terms You May Hear
Subconcussive Head Trauma
Subconcussive impacts are blows to the head that do not cause obvious concussion symptoms but still involve force transmitted to the brain. A person may not feel dizzy, confused, or nauseated — yet the brain still experiences movement inside the skull. Over time, repeated subconcussive impacts may contribute to cumulative brain changes.
Repetitive Mild Traumatic Brain Injury
This occurs when someone sustains multiple mild TBIs over a period of time. Each injury may seem minor on its own, but repeated concussions — especially before full recovery from a prior one — significantly increase the risk of prolonged symptoms and long-term neurological complications.
Post-Concussive Syndrome (PCS)
Post-concussive syndrome refers to symptoms that persist weeks or months after a concussion. These can include headaches, brain fog, sleep disturbance, irritability, memory issues, and sensitivity to light or noise. For some individuals, PCS can disrupt work, relationships, and daily functioning long after the initial injury seemed to “heal.”
Chronic Traumatic Encephalopathy (CTE)
Chronic traumatic encephalopathy is a progressive neurodegenerative disease associated with repeated head trauma. It has been most commonly studied in athletes and military veterans exposed to repetitive impacts. CTE may be linked to long-term cognitive decline, mood disorders, behavioral changes, and dementia. While research is ongoing, repeated brain trauma is considered a significant risk factor.Symptoms Are Different for Everyone
Traumatic brain injuries do not look the same from person to person.
One of the most misunderstood aspects of a traumatic brain injury is that there is no single “look.” Two people can experience the same type of impact and walk away with very different symptoms. Some struggle immediately. Others notice changes gradually over days or weeks. Some symptoms are obvious. Others are subtle but deeply disruptive.
A TBI can affect nearly every aspect of daily life, including:
Physical functioning
- Headaches
- Nausea
- Dizziness
- Sensitivity to light or noise
Thinking and memory
- Brain fog
- Difficulty concentrating
- Slowed processing
- Memory problems
Emotional and social regulation
- Irritability
- Anxiety
- Mood swings
- Depression
Sleep
- Trouble falling asleep
- Sleeping too much
- Restless or disrupted sleep
“Normal” Imaging Doesn’t Mean Normal Brain Function
Brain injuries do not always announce themselves dramatically. Sometimes they show up in the small, cumulative ways that make ordinary tasks harder than they used to be. Persistent headaches, cognitive fatigue, memory lapses, mood changes, sleep disruption, and difficulty concentrating can quietly alter a person’s daily life, career trajectory, and relationships.
In both medical care and litigation, it is critical to evaluate the person — not just the picture. Standard imaging such as CT scans and even many MRIs are designed to detect structural damage — bleeding, fractures, swelling, or obvious lesions. A mild traumatic brain injury, however, often involves microscopic cellular injury, metabolic disruption, and chemical changes that do not appear on routine imaging studies. The brain can be functionally impaired even when it appears structurally intact.
That means a “normal” scan does not necessarily mean the brain is functioning normally. Difficulties with concentration, memory, processing speed, emotional regulation, and sleep can persist despite imaging that looks reassuring on paper. This disconnect between what a scan shows and what a person experiences is one of the primary reasons mild TBIs are frequently misunderstood or minimized.
If you were told in the emergency room that your imaging was normal but you continue to experience symptoms consistent with a concussion, do not ignore them. Follow up with your primary care provider or request referral to a neurologist, concussion clinic, or other specialist experienced in traumatic brain injuries. Keep a written record of your symptoms, note any changes in mood or cognition, and seek further evaluation if symptoms persist or worsen. Persistent symptoms deserve attention — even when the initial scan did not show visible damage.
A brain injury does not have to be catastrophic to be life-altering. Even subtle cognitive or emotional changes can affect work performance, relationships, confidence, and long-term health.
If you suspect a traumatic brain injury, seek medical care. Follow up. Ask questions. Document what you are experiencing. And do not allow normal imaging or outside skepticism to silence your concerns.
The Long-Term Risks
What may be dismissed as “just a concussion” is not always minor. The initial symptoms may fade, but the underlying brain changes can carry long-term consequences.
Moderate and severe traumatic brain injuries have long been recognized as significant risk factors for serious neurodegenerative conditions, including:
- Alzheimer’s disease
- Parkinson’s disease
- Amyotrophic lateral sclerosis (ALS)
What is more concerning is that recent large-scale epidemiological studies have also identified mild traumatic brain injury as a risk factor for dementia.
From a legal perspective, this matters. The value of a brain injury case is not determined solely by the emergency room visit or whether imaging appears “normal.” It includes the cognitive, emotional, and functional changes that follow and the increased risk of future complications. When a traumatic brain injury affects how a person thinks, works, sleeps, or interacts with loved ones, those impacts must be fully understood and properly evaluated in any injury claim.
Early Treatment Matters
The encouraging reality is that many complications associated with a mild traumatic brain injury can be minimized — and in some cases avoided — through early recognition, careful monitoring, and appropriate medical care. Prompt evaluation does more than support recovery; it ensures that symptoms are properly documented and treated before they worsen.
Early medical attention is essential not only for your health, but also for protecting your legal rights. In South Carolina injury cases, clear documentation of symptoms, follow-up care, and physician recommendations can play a significant role in establishing the full impact and value of a brain injury claim.
Guidance from the CDC
The Centers for Disease Control and Prevention (CDC) provides comprehensive, evidence-based guidance for individuals who may have experienced a traumatic brain injury.
Their resources explain:
- Symptoms to watch for
- When to seek emergency medical care
- What to do in the first few days after an injury
- How TBIs are tested and evaluated
- Treatment options
- What to expect during recovery
If you or a loved one has experienced a blow to the head — especially after a car crash or fall — reviewing this guidance can help you recognize warning signs and make informed decisions about medical care.
You can review the CDC’s full guidance here:
👉 https://www.cdc.gov/traumatic-brain-injury/site.html#gen
How We Approach Traumatic Brain Injury Claims
The bruises fade. The vehicle is repaired. On the surface, it may appear that the incident is behind you. But headaches persist. Focus is harder than it used to be. Sleep changes. And sometimes the people closest to you quietly say, “You’re just not yourself.”
When a traumatic brain injury becomes part of a legal claim, it cannot be evaluated based solely on emergency room records or imaging reports. It requires careful review of medical records, follow-up care, symptom progression, and the ways the injury affects daily functioning.
Your brain governs everything you do — how you think, how you feel, how you function. Even subtle changes can influence work performance, relationships, and long-term well-being.
Our approach is deliberate and thorough. We work to ensure the injury is fully documented, properly understood, and accurately reflected in the legal claim — so that the focus can remain where it belongs: on your health and recovery.
Categories
Bicycle Accidents Boating Accidents Bus Accidents Car Accidents Child Injuries Drunk Driving And Other Punitive Issues Food Poisoning Get To Know Us Head Injuries Insurance Motorcycle Accidents Pedestrian Accidents Personal Injury Premises Liability Prescription Drug Overdose Products Liability Property Damage Slip and Fall Accidents Traumatic Brain Injury Trucking Accidents Wrongful Death